Phalloplasty / Female to Male Surgery (FTM Bottom Surgery)
Female to male gender affirmation surgery changes the appearance of female genitals to that of a male's. This has a profound and confirming effect on trans men as they are able to have the body that they were meant to have: Can urinate standing up and can achieve erections with many procedures, will no longer have a vagina, and if a hysterectomy is performed, will also no longer menstruate.
There are two main methods for creating a new penis. These include changing the clitoris into a penis or using a skin flap from the patient's forearm or thigh to create a penis. A person will typically have taken male hormones for at least a year before undergoing either type of surgery. During the procedure, the surgeon also removes the vagina in a vaginectomy, and a hysterectomy is often performed at the same time.
What is Phalloplasty?
Phalloplasty is a surgical procedure in which a penis is created. During the procedure, surgeons take one or more "flaps" of skin and other tissues from a donor site on the body, such as the arms, thighs, or abdomen, and use them to form a penis and urethra.
Who is a good candidate for Phalloplasty?
A good candidate is someone who has taken male hormones for over a year, is healthy and has realistic expectations about the surgery & ongoing care that is needed afterwards.
Benefits of Phalloplasty include:
- Patients are more likely to be able to sexually penetrate their partners.
- The phallus is significantly larger than those created through metoidioplasty although sensation is significantly lower.
- People feel that this surgery creates more natural-looking genitalia.
Phalloplasty in Female-to-Male Gender Confirmation Surgery
Candidate for phalloplasty should have qualities as follow:
1. The patient must be at least 20 years of age. Consent from parents or legal guardians is required to complete the surgery for minors under 20 years old.
2. The patient must have continuously taken male hormone for at least one year.
3. The patient must have lived a life as a man for at least one year.
4. The patient must have undergone a psychiatric evaluation and been declared mentally stable and fit by a psychiatrist.
5. The patient must be physically fit.
6. The patient must have undergone mastectomy and total hysterectomy-oophorectomy for at least six months prior to phalloplasty.

Since 1997 Dr Kamol has performed over 10,000 procedures on transgender patients and over 5,000 sex reassignment surgeries (SRS). Recognized and respected throughout the medical community as one of the most experienced surgeons working in gender reassignment surgery in the world Dr. Kamol currently performs more than 500 male-to-female sex reassignment surgeries each year. He is the chief plastic surgeon at Kamol Cosmetic Hospital in Bangkok, Thailand where he leads the team in male-to-female and female-to-male sex transitions and face feminization.
Phalloplasty Techniques
Kamol Hospital offers the options for phalloplasty as the follows:
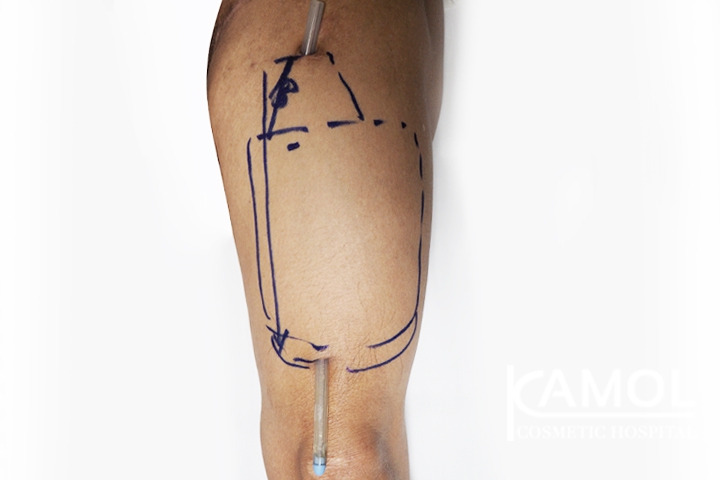
1. Anterolateral thigh pedicle flap (ALT-Phalloplasty)
This is the primary option for phalloplasty in Kamol Hospital.
Due to the individual desire variation, we offer the surgical options for ALT-phalloplasty as follows;
- Full phalloplasty with urethral lengthening: the process starts with prefabricating the urethra The surgery is a two-stage technique with the urethral prefabrication and total vaginectomy for at least 6 months before ALT-flap phalloplasty. The skin with its pedicle containing nerves and vessels from the front and outer part of the thigh is used to reconstruct the new penis. The urethra and sensory nerves are anastomosed at once.
- Phalloplasty with metoidioplasty: in case of metoidioplasty was done earlier, the new ALT-phalloplasty can be done on top of the micropenis. The sensory nerves are shared with the micropenis and the ALT penis. The patient can be standing to urinate through the micropenis at the base of the ALT penis. With this technique, the patient does not take a chance on urethral issues such as urethral stricture or urethral fistula.
- Phalloplasty without the urethral lengthening: this is the most simple phalloplasty without urination concerns. The surgical scar is at the bottom of the penis and the patient urinates through the original urethra
- This is a non-vessel anastomosis technique, thus the risks of vascular thrombosis are very low
Donor skin preparation and the options for the ALT phalloplasty;
- The patient should have hair removal at the front and side of the thighs to avoid the hair growing at the shaft of the new penis.
- The thigh skin thickness must be thin to avoid an oversize penis. Skin fold at the mid-front thigh must be less than 1.5 cm. In case of the thick thigh skin, the patient needs to lose weight, exercise, or have liposuction before surgery.
- The donor site at the thigh is covered with a split-thickness skin graft from the adjacent area.
- In case of avoiding the skin graft, the patient may have the pre-expanded ALT-phalloplasty with the tissue expansion technique. In this technique, the patient needs to stay 1-2 months for the thigh skin expansion before the flap surgery.
- The vaginectomy, hysterectomy, and oophorectomy must be done at least 6 months before the penile reconstruction.
References
- van der Sluis WB., Ronkes BL., Steensma TD., Al-Tamimi M., van Moorselaar., Bouman BM., Pigot Garry LS. Comparison of surgical outcomes and urinary functioning after phalloplasty with versus without urethral lengthening in transgender men. Int J Trans health. https://doi.org/10.1080/26895269.2022.2110548
- Colebunders SD., Stillaert F., Monstrey S. Pre-expanded Anterolateral Thigh Perforator Flap for Phalloplasty. Clin Plast Surg. 44(1):129-141. https://doi.org/10.1016/j.cps.2016.08.004
Advantages of ALT Phalloplasty:
- Good skin color match
- Larger girth than RFF Phalloplasty
- Some natural rigidity
- Less obvious donor site, concealable with clothing
- Decreased surgical time with Pedicled ALT
- Good sensation
- Good potential for urethroplasty
Disadvantages of ALT Phalloplasty:
- More difficult in patients with thicker skin and more subcutaneous thigh fat
- In some patients, girth can be excessive
- Less predictable perforator layout adds complexity
- Sensation is reportedly less than RFF Phalloplasty
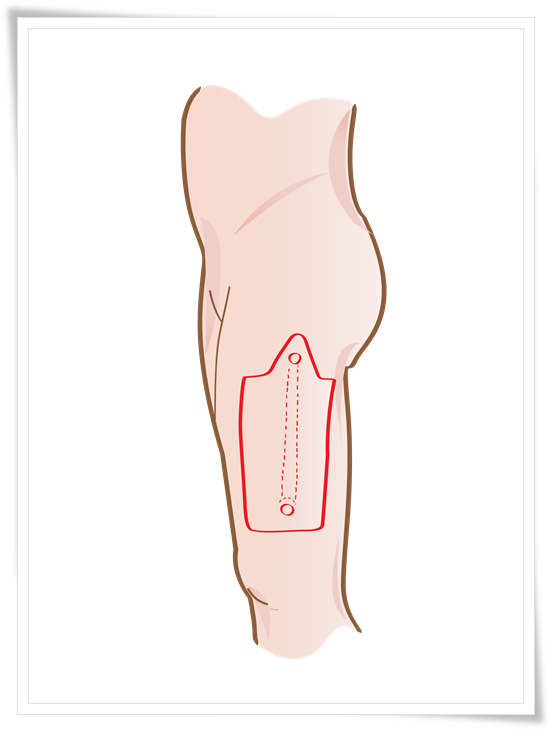
Picture 1: ALT-Pedicle Flap
2. Alternate options of phalloplasty in Kamol hospital
2.1 Radial forearm free flap (RFF): The skin at the front side of the forearm is used to reconstruct the new penis under the microsurgery technique.
Radial forearm free flap (RFF) technique:
We provide two techniques, as follows;
A. Two-stage technique: The two-stage radial forearm free flap technique involves urethral prefabrication prior to themain step (phalloplasty) for six months. This is suitable for those who have small size of forearm.
B. One-stage technique: The one-stage radial forearm free flap involves reconstruction of the neo penis and neo urethra in one stage under microsurgery technique.
Advantages of RFF:
- The skin in this area tends to be thinner.
Disadvantages of RFF:
- Donor site can be difficult to conceal.
- Partial skin graft loss
- Decreased sensitivity,
- Possible motion issues with the hand
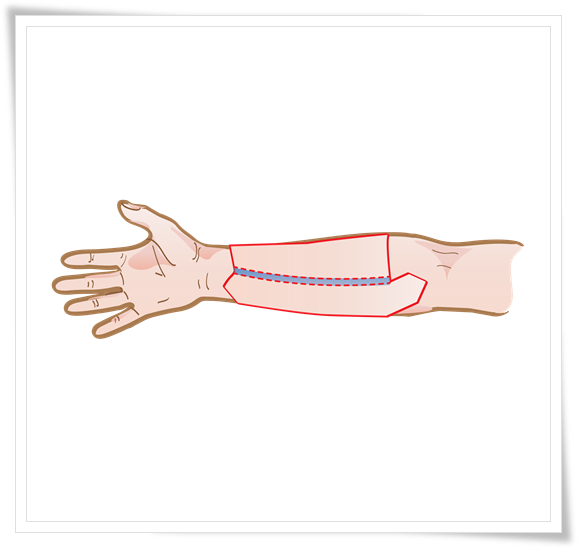
Picture 2: Radial Forearm Free Flap
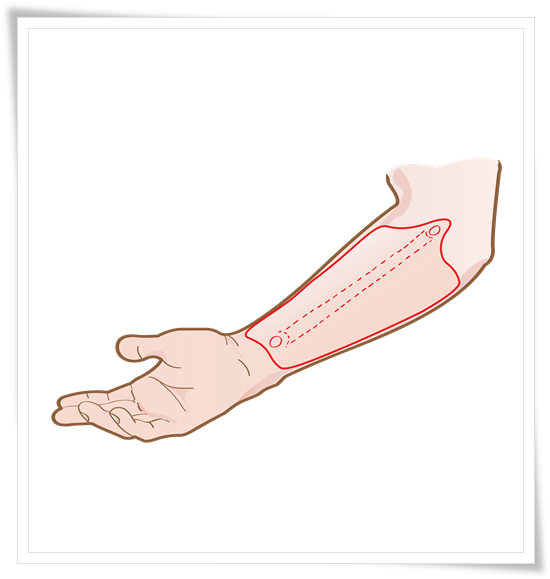
Picture 3: Radial Forearm Free Flap
2.2 Fibula Free Flap (FFF):
The skin, nerves, and some parts of the fibula bone are used as the neophallus (penis) under the microsurgery technique.
Fibula free flap (FFF) technique:
The skin, a piece fibula bone, and nerves are used for the neo penis in one stage under microsurgery technique. The neo urethra is being pre-laminated in situ for six months prior to the main step of neo penis reconstruction.
Advantages of FFF:
- Length of the flap's blood supply
- Less prominent scarring;
- Natural rigidity for penetration with the use of the fibula bone
Disadvantages of FFF:
- Rigid appearance of the phallus.
- Potential bone resorption
- Potential curving and fracture of autologous bone transplants
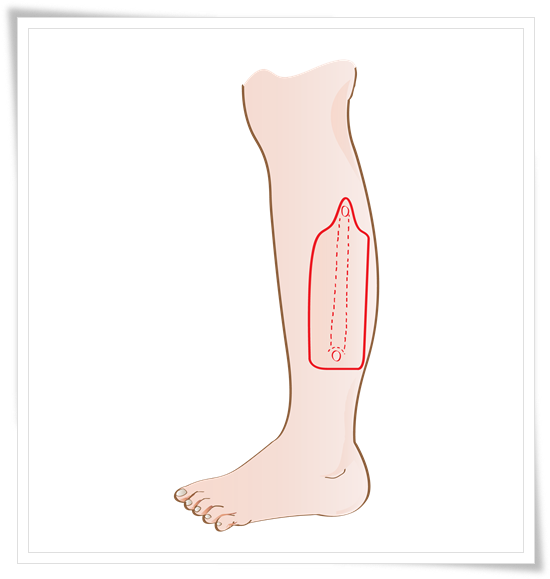
Picture 4: Fibula Free Flap
2.3 Musculocutaneous Latissimus Dorsi (MLD) flap:
The skin island containing nerves and vessels is moved to the genital area to reconstruct the neo penis under the microsurgery technique.
Musculocutaneous Latissimus Dorsi (MLD) free flap technique:
The skin paddle contained nerves and vessels is moved from the area behind the arm to the genital area under the microsurgery technique to reconstruct the neo in the first stage. The neo urethra is constructed the second stage
Advantages of MLD:
● Less conspicuous donor site.
● Relatively hairless donor site
● Good aesthetic outcomes.
● Possibilities for penetrative sex.
Disadvantages of MLD:
● Poor sensitivity of the phallus
● Phallus can be large requiring additional debulking procedures
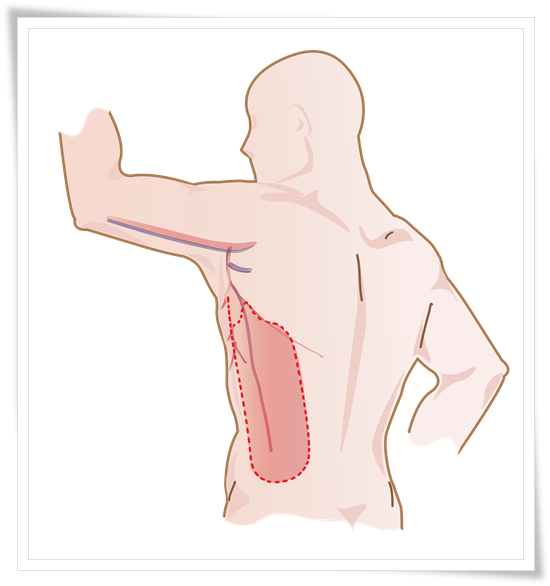
Picture 5: Musculocutaneous Latissimus Gorsi (MLD)
Urethral reconstruction of phalloplasty
Comparison of different phalloplasty techniques
|
Flap technique |
Size of neo penis |
Donor scar |
Sensation |
Self-stiffness |
|
ALT |
Medium-to-Large |
Thigh |
Yes |
No |
|
MLD |
Medium-to-Large |
Side of Torso |
Yes |
No |
|
Radial forearm |
Small -to-medium |
Forearm |
Yes |
No |
|
Fibula |
Small |
Leg |
Yes |
Yes |
After a phalloplasty procedure, it is important for the patient to follow their surgeon's postoperative care instructions carefully in order to minimize the risk of complications and optimize the healing process. This may include taking medications as prescribed, keeping the incision site clean and dry, and avoiding strenuous activities. In some cases, physical therapy may be recommended to help improve the function of the newly constructed penis.
1. Infection: As with any surgery, there is a risk of infection following a phalloplasty procedure. This can be serious and may require additional treatment, such as antibiotics.
2. Bleeding: There is also a risk of bleeding during or after the surgery. In some cases, this may require a return to the operating room to control the bleeding.
3. Scarring: Scarring is a common complication of phalloplasty. The extent of scarring will depend on the specific technique used and the patient's individual healing process.
4. Problems with skin flaps: The skin flaps used to construct the penis during a phalloplasty procedure may not heal properly or may not have a satisfactory appearance. In some cases, additional surgery may be needed to correct these issues.
5. Nerve and blood vessel damage: There is a risk of damage to the nerves and blood vessels in the area during a phalloplasty procedure. This can result in decreased sensitivity or impaired blood flow to the newly constructed penis.
6. Failure to achieve desired results: It is important for patients to have realistic expectations about the outcome of a phalloplasty procedure. In some cases, the results may not be as expected, and additional surgery may be needed to achieve the desired outcome.
Getting to Know for Phalloplasty Surgery:
Detransitioning MTF to Male
Detransitioning MTF to Male
ALT vs MLT
ALT vs MLT
ALT Phalloplasty without urethal
ALT Phalloplasty without urethal
Video: Testimonials of Phalloplasty
ALT Phalloplasty Reviews
Why Kamol Cosmetic Hospital is popular for Phalloplasty?
Kamol Hospital is a popular choice for phalloplasty surgery due to several reasons, including its expertise and experience, state-of-the-art facilities, comprehensive pre- and post-operative care, patient-centered approach, and reputation for excellence in gender affirmation surgeries
Expertise and Experience:
One of the key reasons why Kamol Hospital is popular for phalloplasty surgery is the expertise and experience of its surgical team. The hospital has a team of highly skilled and experienced surgeons who specialise in gender affirmation surgeries, including phalloplasty. They have performed numerous successful surgeries, and their expertise in this field is widely recognized.
State-of-the-art Facilities:
Another factor that makes Kamol Hospital popular for phalloplasty surgery is its state-of-the-art facilities. The hospital is equipped with modern and advanced surgical equipment and facilities that ensure the highest level of safety and quality of care for patients. The hospital also has advanced imaging technology to aid in surgical planning and patient education
Comprehensive Pre- and Post-operative Care:
Kamol Hospital provides comprehensive pre- and post-operative care to ensure that patients receive the best possible outcome and experience. Before surgery, patients undergo a thorough medical evaluation and counselling to ensure they are physically and mentally prepared for the surgery. After surgery, patients receive follow-up care, including counseling and support services, to aid in their recovery.
Patient-Centered Approach:
Kamol Hospital takes a patient-centered approach to care, meaning that they work closely with patients to understand their individual needs and preferences, and tailor the treatment plan accordingly. The hospital's staff is highly trained to provide compassionate care, and they prioritise patient comfort and satisfaction throughout the treatment process.
Reputation:
Kamol Hospital has built a reputation for excellence in gender affirmation surgeries, including phalloplasty. Many patients who have undergone surgery at Kamol Hospital have shared positive feedback and experiences, which has contributed to its popularity. The hospital's commitment to patient-centered care, state-of-the-art facilities, and experienced surgical team have earned it a reputation as a top choice for phalloplasty surgery.
Why Thailand is a plastic surgery destination?
Thailand is a top destination for plastic and cosmetic surgery, as it is the high quality and specialist skills of the surgeons, they provide first-class hospital treatments, and the affordable cost all add up to a satisfying all-around package. There is also the added temptation to recover post-procedure in luxury hotels or recovery service apartments